Is Weight the Problem?
If you have Polycystic Ovary Syndrome (PCOS), you have likely been told to lose weight. If you are trying to get pregnant with PCOS, I have no doubt you’ve been told to lose weight. The typical recommendation from doctors is to lose 5-10% of your total body weight.
The truth is, it’s not all about losing weight. I’d argue that it’s the behavior changes that help weight loss happen that actually drive most of the benefits for fertility.
Research has shown that weight loss improves insulin resistance. We also know that eating more protein improves insulin resistance, exercising improves insulin resistance, and getting adequate sleep improves insulin resistance. So is it losing weight or is it the improvement in insulin resistance? Is it the behavior changes?
In truth, it’s likely all of the above. As insulin resistance improves we see ovulation rates improve. Meaning, you can ovulate more frequently and for some of us - for the first time. Improvements in insulin sensitivity also improve egg quality.
When a PCOS woman does get pregnant, if she has worked to address things like insulin resistance in the pre-pregnancy period we see a lowering of other risks(high blood pressure, preterm birth, gestational diabetes, and preeclampsia.)
We all know the point isn’t getting pregnant. It is about having a baby and living a long healthy life with your family. There are lifelong benefits to lowering insulin resistance and reaching a healthy weight like improved emotional health and lowered risks of diabetes or heart disease. (1)
What does it look like when someone with polycystic ovary syndrome seeks medical help for fertility?
The typical woman receives her PCOS diagnosis and then is offered birth control pills until she is ready to conceive. The doctor says something like, "here is a prescription for birth control and metformin, come back when you are ready to get pregnant. Then we will give you a different medication."
You show back up to the doctor after coming off birth control. Most of the time you haven't had a period and are concerned. You are probably also frustrated, because not having a period may have convinced you that you were pregnant, an additional heartbreak to endure in this process. Next, you see the doctor and they say "try for a year and come back. In the meantime lost 5-10% of your body weight."
If you weigh 200 pounds or 90 kg they will be suggesting 10-20 pound weight loss(4.5-9 kg). That can feel like a heavy burden at the beginning of a fertility journey. Why is this being recommended?
Why are polycystic ovary syndrome patients recommended to lose 5-10% of their body weight?
Often losing weight is a requirement for fertility treatments. When moving on to assistive reproductive technologies like IUI and IVF, some data suggests being at a healthy body weight can improve outcomes. This is incredibly frustrating if it feels like weight is once again an obstacle that you have battled your entire life and is now standing in between you and motherhood.
I hear stories every day that doctors are simply prescribing weight loss and ushering patients out the door.
“To ovulate and get pregnant you need to lose 20 pounds”.
First of all that is likely something you have already tried to do in your life and perhaps failed at. It also isn't very helpful. It would be nice if that statement was followed with a scientifically based way to achieve weight loss.
Have you had an appointment like that? I absolutely did and found myself discouraged and frustrated after the encounter.
As a dietitian, someone with polycystic ovary syndrome, and an infertility patient myself, I had to dig into the research. Now don't shoot the messenger but, there is a good reason for the weight loss recommendations. However, when the main focus of a doctor visit becomes all about weight loss, you can feel helpless and likely were given very few resources on how to accomplish the necessary weight reduction.
What evidence is there for preconception weight loss for women with PCOS?
It has long been known that weight loss can improve metabolic factors with PCOS, particularly insulin resistance.(2) As insulin levels decrease it has a number of beneficial impacts on sex hormones. Testosterone levels decrease significantly as insulin levels decrease. There are many hormonal benefits, but they all trickle down to improved ovulation and egg quality.
Much of this research is done in PCOS populations with a body mass index greater than 25.0. It is undeniable in the research that reproductive outcomes decrease as BMI increases. This isn't to say you can not conceive at a higher BMI or that the pregnancy is doomed from the start, but there is a correlation between excess weight and lack of ovulation and poor pregnancy outcomes.
Most women with polycystic ovaries have a higher body mass index (BMI). Thus, it has basically become second nature for doctors to begin interventions with weight loss recommendations. This is also something they see as beneficial to treat symptoms and overall health. It is also a fairly safe recommendation as they send you out the door to "try" for a year before they will even begin a thorough fertility workup.
Weight Loss for Ovulation
One of the main focuses of fertility treatment for women with PCOS is ovulation induction. That's just a fancy way of saying "getting you ovulating". Women with PCOS typically do not ovulate at all or ovulate very infrequently, sometimes only 2-3 times annually. Since many doctors will not even consider a fertility workup until trying for a year, it is often a complete waste of time if you aren't even ovulating.
In a 2016 secondary analysis of two randomized clinical trials (solid scientific studies), they considered the use of clomiphene citrate (Clomid) on obese PCOS patients trying to conceive. They compared using the ovulation induction medication Clomid immediately or allowing a period of time for participants to implement lifestyle and dietary changes for weight loss. (3)
Now when you consider a study like this it is interesting to look at the outcomes. We don't just want ovulation, we want pregnancy. We don't just want pregnancy, we want live births. No one is trying to get pregnant to miscarry. This study set out to assess these outcomes. Here is a poignant quote from the text:
"One of the striking findings of this study is the marked improvement in live birth rates, out of proportion to the more modest, but still significant improvement, in ovulation rates, suggesting yet again that improving the quality of ovulation is as important as improving the frequency of ovulation."
Was it the weight or something else?
One interesting thing this study set to compare was if being on oral birth control pills during a period of pre-conception improved parameters alone or was the lifestyle and dietary interventions impacted outcomes. It was clear in the study that weight loss was the factor that improved outcomes and suppressing sex hormone production with oral birth control pills was not. (3)
The Amount of Weight Lost Matters in Obese Women with PCOS
Studies show weight loss of fewer than 11 pounds or 5 kg in obese women with PCOS does not yield enough metabolic change to impact fertility. However, in my work with women with PCOS, I have seen incredible improvement in cycle regulation and ovulation regardless of the weight of the individual with a healthy diet, regular physical activity, and circadian rhythm support.
After working with hundreds of women I also can't deny how these things typically improve with weight loss too. I would argue that it is not merely weight reduction, but hormonal improvements associated with behavior change AND weight reduction that really make all the difference.
If this is true why are we being told to lose 5-10% of our body weight instead of being told to improve our overall health? One reason is it’s an easier metric to track. We actually have research showing moderate weight loss like 5-10% of your body weight can improve ovulation rates, pregnancy rates, and live birth rates.
That isn’t to say that if you lose 4% you will not have benefited from it. It just means that around 5% we can see this translate into statistically significant changes. The benefits you are gaining from all the work and diligence you’ve been putting in will remain helpful. Focus less on the percentage or specific number and focus more on the big picture. Working on proper nutrition, exercise, and hormone balance- the weight loss will be an added bonus, you got this!
Before we move on to what to focus on, I want you to understand some of the science behind insulin resistance and hormones. How they interact and why they are the real GOAT when it comes to improving fertility with polycystic ovary syndrome.
How does weight affect insulin resistance?
70-90% of us with PCOS have insulin resistance. So it’s likely part of the puzzle for you too. Insulin resistance is a main player in stopping ovulation from happening. (4) While the entire body becomes insulin resistant, the ovaries do not. They receive insulin's message that energy is available to open the "cell doors" and let it in. In fact, since they aren't insulin resistant, they get A LOT of that message.
This may seem good, let’s get a bunch of eggs ready to ovulate, but it actually turns the little eggs into testosterone-producing power-houses. This is not good for ovulation. We want the immature eggs to be focused on creating more estrogen. Instead, the excess testosterone can stop the eggs from developing. This stops ovulation in its tracks.
Let’s zoom out of the ovary and take a look at how insulin resistance impacts the rest of the body. Insulin resistance means that the rest of the tissues in the body are bombarded by insulin but are actually starved for energy. When our body thinks it’s starving, it makes us super hungry! But the joke is on us, there’s actually a good amount of glucose available in the blood, but we just can’t use it.
There are many reasons those with PCOS experience higher levels of insulin resistance(genetics, age, exposure to plastics, diet, and lifestyle all play a piece). When it comes to this recommendation from doctors though, we do know that extra amounts of fat tissue (and higher levels of testosterone) all make insulin resistance worse. So there is merit to recommend weight loss to improve these metabolic factors that impact ovulation.
Insulin resistance improves with weight loss. When weight loss occurs insulin resistance goes down. No matter which is the chicken and which is the egg, both can improve ovulation rates. Both can also cause the other to occur.
What Hormones Related to Fertility Improve When A PCOS Woman Loses Weight?
Alright, here's the deal. Having excess insulin results in the body trying to correct itself. It does this by producing more testosterone as mentioned above(5). Not to throw more fuel on the fire but it’s not just testosterone stalling ovulation. Follicle-stimulating hormone (FSH) and luteinizing hormone (LH) stop being released at optimal levels from your brain. These two hormones are critical for helping a follicle (or egg) develop and be released from the ovary.
In PCOS it’s very common for LH to be higher than it should be. LH is responsible for telling your body WHEN to release an egg. If it is always high, there is no way for it to create a large peak (or surge) and signal the ovary to release an egg.
The exact ratios between FSH and LH matter as a delicate balance is necessary to make an egg mature and be released from the ovary. Insulin resistance can draw these hormones out of balance. This results in less-than-ideal egg quality or complete cessation of ovulation.
When estrogen production is low (remember how too much testosterone means lower estrogen) your body will make less cervical mucus. This is important because one of its primary roles is to keep sperm alive in your vagina's acidic environment. Less cervical mucus means sperm have a more difficult time reaching an ovulated egg. It also gives less of a preview as to when sex timing is most optimal.
Hormone imbalances related to insulin resistance do not stop there: progesterone also has important roles in your fertility. Even if you are ovulating, if your body struggles to make enough progesterone it will be difficult to hold a pregnancy or prepare the uterine lining for implantation. Insulin resistance can impact the body's ability to make progesterone. With all of this hormonal disruption, if ovulation does happen, the egg quality is less than ideal and fertility suffers.
Wow, that’s a lot to take in. Here’s the good news, by simply focusing on improving insulin resistance we are indirectly improving our fertility by regulating all those hormones. So, don’t feel discouraged, you got this!
As an aside, I just wish we could start calling "male hormones" huntress hormones instead. Men are not the only ones that make these, and PCOS women just make too much of them.
What if I have lean PCOS? What if I don't need to lose weight?
Lean polycystic ovarian syndrome has become a term used to refer to anyone with PCOS that has a BMI of 25.0 or lower. A normal BMI is in the range of 18.5-25.0. Essentially it is anyone with a 'normal body weight'(BMI of 18.5-25.0) or even a 'low body weight' (a BMI under 18.5).
The common misconception with the medical treatment of those with "lean PCOS" is that they do not experience insulin resistance like those that struggle with excess weight as a symptom. This could not be further from the truth.
When comparing lean PCOS individuals with weight and age-matched controls that did not have a PCOS diagnosis, it was shown that the PCOS patients had higher levels of insulin. Some reports estimate 60-70% of lean PCOS individuals struggle with insulin resistance, others a lower figure of 20-25%.
Since we know higher levels of insulin are shown in lean PCOS individuals- it's important to remember the insulin mechanism of action on the ovary is to increase testosterone and impact ovulation. Insulin also impacts the brain in the pituitary to signal higher levels of LH - which can greatly stall ovulation.
Yet, a lean individual with PCOS likely should not be counseled to lose 5-10% of their body weight. So what should a lean individual do to improve fertility? Regardless of weight status, focusing on blood sugar balance will support healthy hormone signaling for ovulation.
The lean PCOS population appears to struggle more significantly with adrenal gland hormone production of androgens, specifically DHEA-S. DHEA-S can stall ovulation just like testosterone can. High levels of DHEA-S can also impact other health problems like inflammation and irregular periods.
Whether someone struggles with excess weight as a PCOS symptom, even moderately elevated levels of insulin can increase male hormones disrupting ovulation and fertility. You do not need to suffer from metabolic syndrome to see hormonal imbalances with PCOS. Do not let a normal weight feed a narrative that diet is not impacting your fertility problems.
What if it's not Lean Polycystic Ovary Syndrome (PCOS)?
Sometimes individuals will be diagnosed with PCOS and told they have "Lean PCOS" when they actually have Hypothalamic Amenorrhea (HA). Hypothalamic amenorrhea is a condition similar to PCOS in that the menstrual cycle is affected. Ovulation is typically shut down and pregnancy is difficult to attain.
While both PCOS and HA are diagnosed with the help of cycle history and both typically involve anovulation, they have completely different causes disrupting a woman's fertility.
Hypothalamic Amenorrhea is a condition characterized by inadequate energy consumption. This could be due to under-eating, over-exercising, or both. Many health providers do not consider HA unless an individual is "under-weight" however you can experience HA at any body weight if the body is not adequately nourished. It then lacks the needed resources to be available for reproduction.
If you are reading this and considering the question, 'do I have PCOS or HA', I'd invite you to listen to a podcast that was recorded with Lindsey Lusson called: Do I have HA or PCOS?
If you believe your Lean PCOS is a misdiagnosis and you may actually have HA, weight loss will be the EXACT WRONG THING TO DO to get pregnant. What individuals need who are struggling with anovulation due to inadequate energy intake is MORE CALORIES.
How Does Weight Loss Impact Pregnancy Outcomes?
In addition to regulating hormone production, losing excess fat will benefit you once you do conceive. Earlier in this article, we discussed a study that showed weight loss preconception increased live birth rates. It also improves pregnancy outcomes. Pregnancy is a natural process, beautiful, and sacred. Entering pregnancy as healthy as possible can provide advantages in pregnancy outcomes and the health of the baby.
We do see weight loss decrease chances of pregnancy complications such as gestational diabetes, gestational hypertension, pre-term birth rates, and pre-eclampsia. Again it's likely the additive effect of improved hormonal balance, healthy eating principles, behavior change, physical activity, decrease in male hormones, and other health conditions and not just weight.
Excess weight is linked to many diseases including diabetes and heart disease. (6) I guess the not-so-specific weight loss recommendation is still frustrating, but now at least you have some context to the ‘why’. If you're interested in how to take the next steps toward lifestyle changes to achieve weight loss (hormone balance), check out the Find Fertility course.
How do I lose weight with PCOS?
In order to lose weight there has to be something called a "calorie deficit". Essentially you need to burn more calories than you are taking in through food and drink. With PCOS it can be difficult to lose weight with hormonal abnormalities. Focusing on improving these hormonal abnormalities with blood sugar balance will assist in weight loss efforts.
What hormonal abnormalities make it more difficult to lose weight with polycystic ovarian syndrome?
The two main hormones that make weight loss an increased struggle with polycystic ovary syndrome are insulin and leptin.
- Insulin has the main function of getting energy where it needs to go in your body. When calories are higher than needed, insulin helps the extra energy gets stored for later. You might be familiar with this concept or tissue, it's called "fat".
When you have insulin resistance, you make more of insulin to get the same message sent - more of that message to "store fat" circulates around your body. It can be increasingly difficult to lose weight when your body is being signaled to store energy as fat for later.
- Leptin is the hormone that tells your body that you are full after eating. Regardless of weight status, women with PCOS have been shown to have leptin resistance. This is difficult for weight loss for a number of reasons, but perhaps most importantly when it comes to appetite. It is difficult to get into a "calorie deficit" when your body is persistently hungry.
Which diet is most effective for weight loss for polycystic ovary syndrome?
The most compelling research for PCOS weight loss that improves ovulation is calorie restriction. More specifically very low-energy diets have been shown to restore ovulation, improve insulin resistance, and help women lose weight. (7) Much of this research has been conducted with small research samples and is done over 12 weeks periods of time or less.
As a dietitian that treats women with PCOS, I see many issues with a very low-calorie diet as the main focus of interventions. When we are considering a group that is trying to conceive and go on to grow an entire human in their womb, I have even more concern.
Moderate calorie restriction with a focused plan designed for blood sugar regulation that increases protein intake, increase fiber intake, and optimizes healthy fats is a formula that can yield weight loss, but also checks off many of the needs for specific nutrients of concern pre-conception. This also is not overly restrictive and focuses on what foods to increase versus vilifying and avoiding many foods.
For a nutrition plan (or diet) to be successful it has to be sustainable. A very low-calorie diet is not sustainable or advisable in pregnancy and thus is not something I would recommend in preconception. Physical activity also improves insulin resistance and can promote ovulation. Exercise can be difficult to continue on a very low-calorie diet.
Should I consider Medication to Help with Weight Loss Preconception?
Common medications used to assist women with PCOS to lose weight include Metformin, Phentermine, Ozempic, Victoza, and Trulicity, among others. (7) Other than phentermine which is an appetite suppressant, the other prescription medications help to improve insulin resistance by a number of different mechanisms. Each of these drugs is used in an "off-label" way. Meaning that it was not designed or approved by the FDA for use in PCOS for weight loss or any reason.
All of these medications have been shown to help achieve weight loss in PCOS individuals. (7) However, not all are compatible with pregnancy and as such may require a "wash-out" period between taking the medication and efforts toward conception.
All of these medications have actually been shown to help ovulation and pregnancy rates. I am a dietitian and will always propose food as medicine. It is my scope of practice. People often assume because I treat things "naturally" I am anti-medicine. That could not be further from the truth.
Some of these medications may be the exact right next step for you. However, you should never go on any medication without a thorough understanding of what it is, how it works, its risks, benefits, and alternatives. This is called "informed consent". It should be the standard of medicine but unfortunately is not.
Medications also come with side effects and these should be considered or at the very least monitored while taking these. It is notable that most of these medications when they are "stopped" result in weight gain.
If employing these medications they need to be taken while working on behavior change, healthy eating, physical activity, etc. You can't just take a pill, lose weight, get pregnant, and expect things to not return to the baseline before the medication.
You should consult your OB/GYN or reproductive endocrinology physician about the potential benefits, risks, and alternatives of these medications for your specific goals. Looking critically at the research employing cognitive behavioral therapy and nutrition education both help someone be the most successful when taking a medication such as these.
Only you can decide what is the best next step with your healthcare providers, partner, and most importantly what feels right to you.
Should I consider Supplements to Help with Weight Loss?
There are many options for supplements that are safe in preconception that will actually improve egg quality, insulin resistance and have been shown to help induce ovulation. As these can help with improving insulin resistance they have also been shown to aid in weight loss efforts.
However, taking these alone will not cause weight loss, you will have to pair it with nutrition and lifestyle changes as well. A few I would consider are:
- Myoinositol
- NAC
- Magnesium
All of these are available in the PCOS Formularies Supplement line. Take this quiz to find the best supplements for your current goals and PCOS symptoms here.
My doctor recommended bariatric surgery as an option, is this safe before pregnancy?
I have seen a trend in doctors recommending bariatric surgery for individuals whose BMI is higher than 40 to help improve overall health, but with a particular focus on the fertility future of the individual. Bariatric surgery is an incredibly invasive surgery that should not be considered lightly.
In fact, it's my opinion that an individual needs thorough assessment by both a dietitian and a therapist before embarking on such a life-changing surgery. All methods of bariatric surgery impact nutrient absorption. This is one of the ways they affect weight loss so profoundly.
I have worked with many PCOS patients after they had bariatric surgery and are considering getting pregnant to help optimize their diet to help ensure nutrient density for healthy preconception and pregnancy nutrition.
I do believe bariatric surgery has its place as an intervention, but should be considered when attempts have been made already and an individual feels this may be the best option given their health history and goals. We have a great amount of research on weight loss surgeries such as these on metabolic outcomes, and the statistics are promising, however - we have NO research in pregnancy and live birth rates for PCOS.
Let me type that again: There are no RCTs that assessed the impact of bariatric surgeries on pregnancy rates and live birth in PCOS. (7) As a treatment modality, it should then be considered on a case-by-case basis with your healthcare professional.
There are other invasive surgeries that can improve fertility with PCOS like ovarian drilling- just like bariatric surgery, I would never consider this as a first-line treatment option.
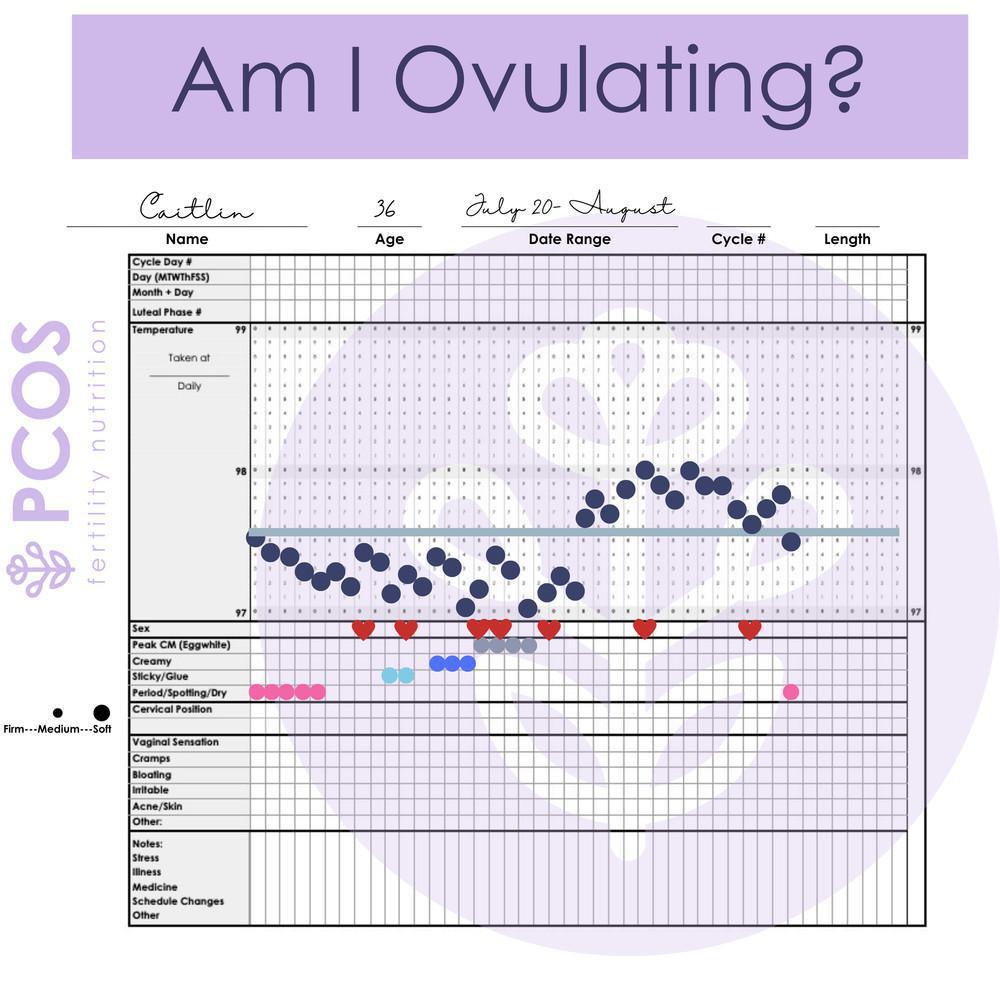
How do I know if I'm ovulating if I have PCOS?
Cervical mucus surveillance, cervical position tracking and basal temperature charting will help you determine if you are currently ovulating. Many women start with cycle-tracking apps or ovulation predictor kits. Your body is smart enough to tell you this without fancy technology. If you want to learn if you are ovulating I created an entire mini-course on this called Cycle Tracking + PCOS.
If you feel like you need some "smart technology" to help you determine if you are ovulating, my favorite cycle-tracking technology is called TempDrop.
Can I get pregnant with PCOS naturally?
Yes! Your fertility future is promising! Many people who work on ovulation induction go on to have healthy pregnancies and children. Weight loss may help you with these goals. However, it's not as simple as the doctor makes it sound, 'losing weight will equal ovulation'.
Optimizing your nutrition, focusing on specific interventions, physical activity, stress management, circadian rhythm support, and ovulation typically occurs without medication because of lowering male hormones.
Many women do go on to get pregnant naturally, or what I like to say is "in the wild". Some will need additonal support to get pregnant. This may mean medication, intrauterine insemination (IUI) or in vitro fertilization (IVF). It may just mean metformin or letrozole or clomid.
No matter your route to conception, focusing on nutrition is an important part of your health, the health of your pregnancy, and future child. Nutrition matters and should be given due attention. I highly recommend anyone with PCOS that is trying to conceive consider joining the next round of my premier course Find Fertility with the PCOS + Method.
Meet baby Eli Micheal.
This is just one of the hundreds of baby's born to PCOS women in my Find Fertility course.
What are my chances of conceiving with PCOS?
I have worked with my fair share of reproductive medicine doctors and many LOVE treating women with PCOS. Why? Because they get pregnant! I love treating women with PCOS for the same reason. PCOS is not an infertility diagnosis. However, it does make it more difficult and likely to take longer for us to get pregnant.
The literature has shown women with PCOS do not have any fewer children than women that do not have this diagnosis. Keep your chin up friend. Don't let a recommendation to lose weight discourage you. It may help the process. Make sure you find support to lead a healthy lifestyle.
Sources
1 Jean Hailes. Weight- Management and Treatment. Retrieved November 2022. https://www.jeanhailes.org.au/health-a-z/pcos/weight-management-treatment#:~:text=Benefits%20of%20weight%20loss%20with%20PCOS,-Even%20a%20small&text=Weight%20loss%20can%20restore%20the,hair%20loss%20and%20menstrual%20regularity.
2 Weight control and its beneficial effect on fertility in women with obesity and polycystic ovary syndrome. https://doi.org/10.1093/humrep/12.suppl_1.82
3 Benefit of Delayed Fertility Therapy With Preconception Weight Loss Over Immediate Therapy in Obese Women With PCOS. https://academic.oup.com/jcem/article/101/7/2658/2810119
4 Legro, R. (December, 2012). Obesity and PCOS: implications for diagnosis and treatment. DOI: 10.1055/s-0032-1328878
5 Silvestris, E. (March, 2018). Obesity as disruptor of the female fertility. DOI: 10.1186/s12958-018-0336-z
6 Best, D. (November, 2017). How effective are weight-loss interventions for improving fertility in women and men who are overweight or obese? A systematic review and meta-analysis of the evidence. DOI: 10.1093/humupd/dmx027
7 How to manage weight loss in women with obesity and PCOS seeking fertility? ttps://onlinelibrary.wiley.com/doi/full/10.1111/cen.14726